Advance Care Planning & DNACPR: reports & publications
The Parliamentary and Health Service Ombudsman report, released in March 2024 and calling for improvement in DNACPR conversations is the focus for this blog. It is an important document highlighting current failures in practice and recommending steps for the way forward.
The dual purpose of this blog is to place the report in context of other relevant and key publications and to highlight the findings of the report.
The first publication to address concerns is Protect, respect, connect – decisions about living and dying well during COVID-19 published in March 2021.
Protect, respect, connect – decisions about living and dying well during COVID-19
The Protect, respect, connect report is a summary of concerns around ‘do not attempt cardiopulmonary resuscitation’ (DNACPR) decisions made during COVID-19. The report presents the concerns specifically about involving people in the decision making and applying decisions to groups rather than individuals.
“What we have found through our review is a worrying picture of poor involvement,
poor record keeping, and a lack of oversight and scrutiny of the decisions being
made. Without these, we cannot be assured that decisions were, and are, being
made on an individual basis, and in line with the person’s wishes and human rights”
Findings from the report demonstrate there needs to be a focus on the following themes:
1. Information, training and support
2. A consistent national approach to advance care planning
3. Improved oversight and assurance
You can read the report in full here.
Universal Principles for Advance Care Planning
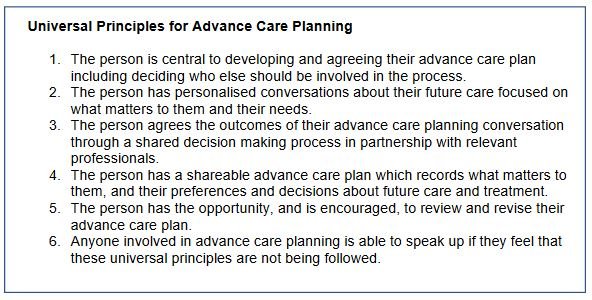
In response to the Protect, respect and connect report the Universal Principles for Advance Care Planning was published in March 2022. The report is a collaboration between NHS England, NHS Improvement and partner organisations and it presents high level principles for Advance Care Planning. The aim of the principles set out in the report are to improve inclusion, equality and diversity in Advance Care Planning.
After describing what Advance Care Planning is, benefits of Advance Care Planning and considerations in practice, the report sets out six universal principles:
You can read the report in full here.
The report closes with a list of seven requisites to achieving good practice in Advance Care Planning:
1. Public and professional awareness
2. Clear information
3. Proactive identification of those who would benefit from ACP
4. Education and training to ensure
5. Record keeping and information sharing
6. Organisational culture
7. System culture
Having looked at the key publications, I will now move to the second part of the blog and highlight findings of End of life care: improving ‘do not attempt CPR’ conversations for everyone published in March 2024.
End of life care: improving ‘do not attempt CPR’ conversations for everyone
The Parliamentary and Health Service Ombudsman is an independent body working to investigate complaints UK Government departments and the NHS in England. The forward to the report includes a summary of challenges and impact around end of life care conversations:
“Conversations about end-of-life care are sensitive and emotionally challenging.
They need to be conducted by professionals who have had appropriate training, in
partnership with patients and their families and supporters. The aim is to help
them make the right decision, properly informed and at the right time. However,
the evidence of this report shows that good practice is missing in some parts of our
healthcare system, and that this can have profoundly traumatic consequences for
patients and their families”
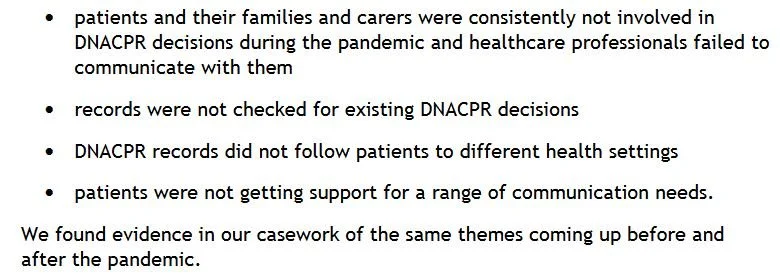
Through casework and research into complaints received about ‘do not attempt cardiopulmonary resuscitation’ a number of flaws in practice were identified. The report states that whilst the problems were highlighted during the pandemic, they are more widespread than that time frame.
The flaws identified show that:
Further case work also informed the report and showed that:
The report presents main findings with case studies powerfully illustrating the human impact of each issue. It is not the intent of this of this blog to present findings in detail but instead to draw attention to the main findings, listed below.
Main findings
Patients and families are not always told about DNACPR decisions
Conversations often happen too late and in emergency settings
DNACPR conversations are often left to family members as patient’s wishes have not been discussed before it is too late
There is a lack of accessible information given at the time or before DNACPR conversations
There are issues with record-keeping and documenting decisions
People voiced genuine fears about ageist and ableist attitudes and behaviours in the NHS
There is a lack of public awareness and knowledge about DNACPR
The report closes with recommendations, summarised here.
Recommendations
Training - to include scenario based training on DNACPR
Communication - to ensure communication is accessible and staff are trained in EoL conversation skills
Regulation - CQC should update guidance and include assessment of provider compliance with DNACPR good practice
Record keeping - aimed at NHS England to ensure advance care planning conversations are accessable and shared
Overarching recommendation – “We call for all outstanding recommendations in CQC’s ‘Protect, respect, connect – decisions about living and dying well during COVID-19’ to be implemented”
Closing reflections
Twitter, (X), activity in the immediate aftermath of publication of the report showed how emotive DNACPR discussions and Advance Care Planning is. I sensed too a feeling of frustration that lessons learned from before remain an issue today. Ordinary Dying remains poorly understood, arguable both by Health Care Professionals and the public, and CPR misconceptions are fuelled by unrealistic media representation. Conversations are happening too late and often during a time of crisis rather than as part of a proactive plan. We need to do better.
I hope the blog is useful in providing a road map of relevant reports and a summary of current issues. I recommend clicking through the links to access further resource and find out more.
If the blog has helped you or provided information and you would like to support my ongoing work, head to Buy me a coffee – thank you!
https://www.buymeacoffee.com/6nqvjqvgly