Can a family create an Advance Decision to Refuse Treatment for someone who has lost capacity?
Can an Advance Decision to Refuse Treatment be written by an attorney? This is the essence of a question I have been asked recently, and will answer in the flowing blog. The person who posed the question kindly consented for me to share an anonymised background and the questions they faced.
Background and questions
Care staff have been proactively engaged in Advance Care Planning with a family of a person who does not have capacity to make some health care decisions. In a local Advance Care Planning booklet there is a section a for an Advance Decision to Refuse Treatment decisions, care staff completed this with person’s daughter who holds Lasting Power of Attorney for Health and Welfare.
· Can a family create an Advance Decision to Refuse Treatment for someone who has lost capacity?
· If not, what would be the best way to document the person’s wishes?
· What does this mean for families who's loved one have lost capacity but they know, for example, that their Mum would not want a PEG feed if in future this was advised?
Before answering the questions, I will set out some of the important terminology and frameworks that are involved; understanding these will help to identify answers to the questions. I will then address each of the questions separately.
What is Advance Care Planning?
Advance Care Planning is a process of discussions enabling a person to consider what their preferences and priorities for future care may be. Advance Care Planning is built on a foundation of What Matters Most to a person, can be started at any stage of life and, I argue, it is Just a normal part of life planning . The output of discussions could result in a number of documents or plans – there is no single way of creating an Advance Care Plan.
It can be helpful to think of Advance Care Planning under the following broad headings and
· What you do want
· What you don’t want
· Who would speak for you
· Your Legacy
· End of Life Care
I explain these in more detail in the blog Advance Care Planning: Getting Your House in Order While the process is called Advance Care Planning, an Advance Care Plan is a document (or combination of documents) that summarises the planning – it may be a local document and it is worth finding out what is used in your area.
What is a Lasting Power of Attorney?
A Lasting Power of Attorney is a legal document that lets you appoint one or more people to make decisions on your behalf. This gives you more control over what happens to you if you have a sudden accident or an illness and cannot make your own decisions. The people you appoint are called attorneys.
There are two different kinds of Lasting Power of Attorney, one for Health and Welfare and one for Property and Finance. A Health and Welfare LPA would be used if you lost capacity to make decisions about issues relating to health (e.g. whether you should have surgery or other medical treatments). An important element of the Health and Welfare LPA is that it offers the opportunity to give the person or people appointed, (the attorney(s)), authority to make life-sustaining treatment decisions.
A Property and Finance LPA is used for to appoint someone to make decisions about your money for things like paying bills, collecting pensions or selling your home and can take effect, with your consent, as soon as it is registered.
To make a Lasting Power of Attorney you must have appropriate mental capacity. The application process requires confirmation from a ‘certificate provider’ that you’re making the Lasting Power of Attorney by choice and that you understand what you are doing.
What does “having capacity” mean?
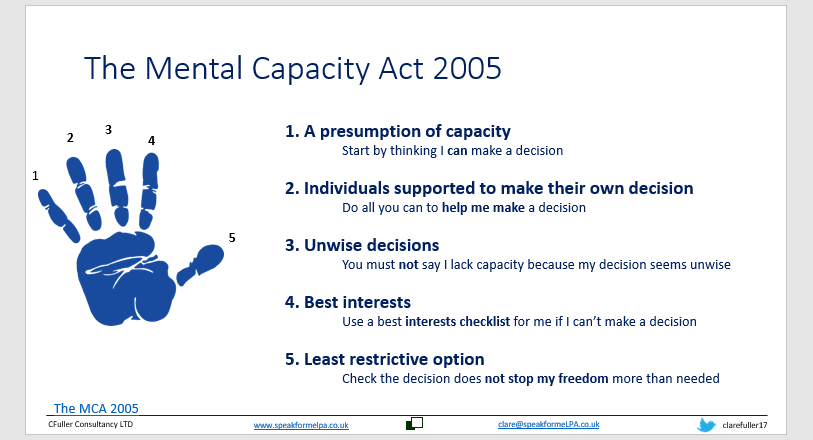
Having mental capacity means having the ability to use and understand information to decide and to communicate any decision made. It is important to remember a person may be able to make some decisions or decisions with support and the Mental Capacity Act 2005 sets out the five principles.
You can listen to an explanation of capacity in the podcast: Mental Capacity: it’s decision specific not a binary concept with Dr Maggie Keeble
What is an Advance Decision to Refuse Treatment?
An Advance Decision to Refuse Treatment (ADRT) is a legal document which sets out specific treatments a person may wish to refuse in the future. To complete an ADRT a person must be over the age of 18 and have appropriate capacity. The document must be signed, witnessed and contain the statement “even if my life is at risk”.
An ADRT identifies a specific treatment that a person wishes to refuse in a specific circumstance and you can read more about ADRTs in the blog Making my Advance Decision to Refuse Treatment
Addressing the questions
Having covered the framework and terminology answers to the questions will now be clearer to navigate.
Can a family create an Advance Decision to Refuse Treatment for someone who has lost capacity?
The simple answer to this is no, a family (or any attorney for health and welfare) CANNOT create an Advance Decision to Refuse Treatment for a person who has lost capacity.
If not, what would be the best way to document the person’s wishes?
To document a person’s wishes we need to know what those wishes would be – it sounds obvious but is worth highlighting here. There would be a number of things to consider. Finding out if the person had documented any preferences or instructions in the Lasting Power of Attorney that could provide an insight into a person’s wishes. In the absence of information in a Lasting Power of Attorney, are there any Advance Statements of wishes and Preferences for the person available? Whist not legal, they are valuable in finding out what is important to a person.
Keeping in mind principles of the Mental Capacity Act, it would be important to support the person to make a decision by providing, for example, information in a way that could be understood.
Lastly, Best Interests decision making would apply. The MCA sets out a checklist to consider when deciding what is in a person’s best interests.
The best interests checklist states you should:
encourage participation – do whatever is possible to permit or encourage the person to take part
identify all relevant circumstances – try to identify the things the individual lacking capacity would take into account if they were making the decision themselves
find out the person's views – including their past and present wishes and feelings, and any beliefs or values
avoid discrimination – do not make assumptions on the basis of age, appearance, condition or behaviour
assess whether the person might regain capacity – if they might, could the decision be postponed?
It's vital to consult with others for their views about the person's best interests.
In particular, try to consult:
anyone previously named by the individual
anyone engaged in caring for them
close relatives and friends
any attorney appointed under a Lasting Power of Attorney or Enduring Power of Attorney
any deputy appointed by the Court of Protection to make decisions for the person
(information from https://www.nhs.uk/conditions/social-care-and-support-guide/making-decisions-for-someone-else/mental-capacity-act/ )
What does this mean for families who's loved one have lost capacity but they know, for example, that their Mum would not want a PEG feed if in future this was advised?
In the specific example given above, relating to PEG (Percutaneous Endoscopic Gastrostomy) feeding, the family have Lasting Power of Attorney for Health and Welfare and can refuse this treatment on behalf of their Mother if they believe it to be in her best interests. This would only be applicable if they have Option A or the ability to make life sustaining treatment decisions under the conditions of the Lasting Power of Attorney.
It is worth noting that a family holding a Lasting Power of Attorney with the relevant powers can refuse the PEG. Their refusal however, can be set aside if others (professionals/judge) consider a PEG to be in their Mother's best interests. [1]
It would be relevant too for discussion to consider why the PEG feeding was indicated – was this a short-term answer for an acute potentially recoverable event or associated with a longer-term chronic illness or disease?
Conclusion
Understanding the Mental Capacity Act and frameworks that support Advance Care Planning is essential in answering the question at the heart of this blog. It is not possible for an attorney to write an Advance Decision to Refuse Treatment for a person who has lost capacity to do this themselves.
This has been a great question to answer, bringing out many key elements of Advance Care Planning and highlighting the importance knowing what really matters most to a person.
If you have a question you would like featured in blog contact me
If the blog has helped you or provided information and you would like to support my ongoing work, head to Buy me a coffee – thank you!
[1] I am grateful to Celia Kitzinger for her comment to clarify this point